Displacement ventilation in a typical office
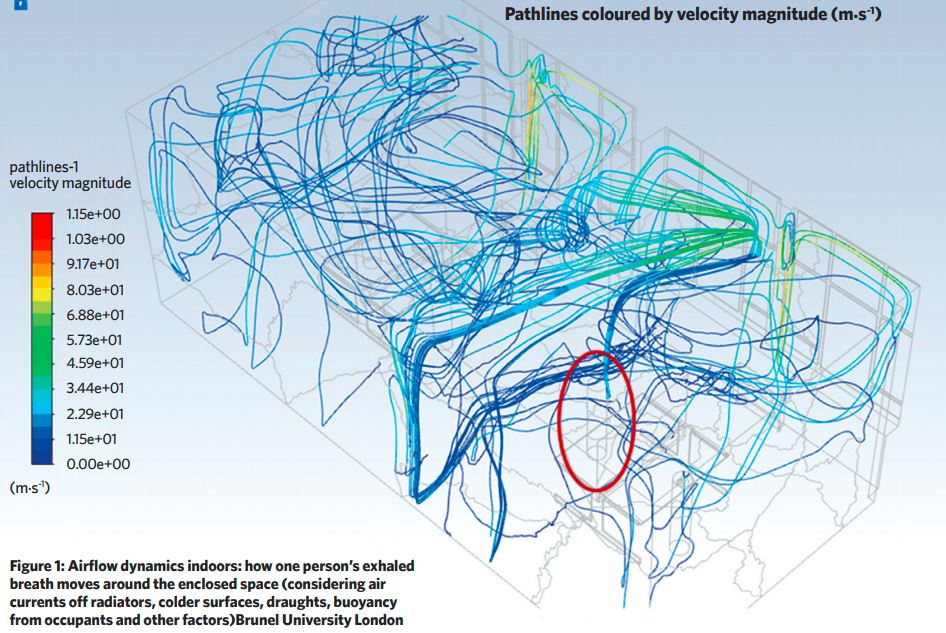
It is hard to write about Covid-19 and cover new ground, but one area that seems to have been almost entirely neglected is airflow dynamics. In the pandemic, ventilation was initially ignored as people followed the World Health Organization’s (WHO) unfounded fomite theory,1 despite mounting scientific evidence against it.2
When the WHO finally admitted that airborne transfer was a possibility (almost nine months after 239 scientists wrote an open letter urging it to accept the airborne route)3 it continued to insist that aerosol transmission was rare, and fomites were key to the spread of infection.4
Technical symposium winning paper
Tom Lipinski’s paper Impact of various ventilation strategies on indoor airflow dynamics and the spread of pathogens such as Covid-19 was presented at the 2021 CIBSE Technical Symposium and was voted as making the most significant contribution to the art and science of building services engineering.
Professor Cath Noakes changed her Twitter handle from #hands #face #space to #ventilate to encourage people to start taking ventilation seriously. Still, unanswered questions remained: is it about air changes per hour? Does how we ventilate matter at all?
We see air changes per hour (ACH) requirements – 10L.s-1 per person, or 15L.s-1, or as much as 210L.s-1 per infected person, for example – thrown around with authority, yet we don’t see much of a discussion about how breath spreads indoors and whether some ventilation methodologies manage this better than others. Interestingly, this debate took place years ago following SARS-CoV-1, with intriguing outcomes.
The fact many super-spreader events happened in settings with good or adequate ventilation should have raised alarm bells immediately. The Skagit Valley Chorale practice that resulted in 53 infections (out of 61 attending) and three deaths, had a modern, forced-air heating and ventilation system installed that was running at 0.7 ACH during the event, designed for occupancy of up to 180.5
The call centre in Seoul, where 94 out of 216 employees were infected, had a functioning, positive pressure HVAC system in place, delivering a recommended airflow rate.6 This inconsistency should have been spotted earlier, but this was happening while the WHO was peddling its unhelpful fomite theory.
How do we ventilate?
There are two main ventilation methodologies (when it comes to airflow dynamics): mixing ventilation and displacement ventilation. Each has had dominance at some point in the past. Despite displacement ventilation previously having a dominant position, it has lost some popularity. This may be because developers have worked out they can save 2% on the build cost if they pack building services into the ceiling void.
You might be old enough to remember sockets, as well as air vents punctuating the carpet under your desk – that was when displacement ventilation ruled.
The objective of mixing ventilation (always mechanical) is to ensure that everyone gets the same quality air, wherever they are in the room. It’s not all fresh though, it is mixed with the room air so everyone in the room breathes elements of other people’s exhaled air.
Displacement ventilation, however, (frequently natural) adheres to the rules of physics, using buoyancy (warmer air rising) to facilitate the removal of stale air. Displacement ventilation needs considered design and architect and engineer to work together, which can be hard.
Mixing ventilation is much easier to implement and manage, needs ducts and fans; and is less demanding on the actual space, opening sizes and the layout.
Most importantly, the way we ventilate seems to matter a great deal when it comes to pathogen spread indoors – not least when considering the impact of coronavirus.
History
None of this, especially with the infection spread in mind, is new. In 2010 Hua Qian et al published a paper titled Natural ventilation for reducing airborne infection in hospitals.7 The researchers conducted real-life tests of various methods used in a hospital ward, complete with thermal manikins and tracer gas (sulphur hexafluoride) to measure air exchange rate.
The authors observed that downward ventilation systems could not produce a unidirectional airflow pattern, since thermal plumes of manikins induced mixing and disturbed pollutant removal, while a higher location for exhausts resulted in more effective pollutant removal from the ward. They concluded that natural buoyancy-driven displacement ventilation was much more effective at removing pollutants than a top-down mixing one.
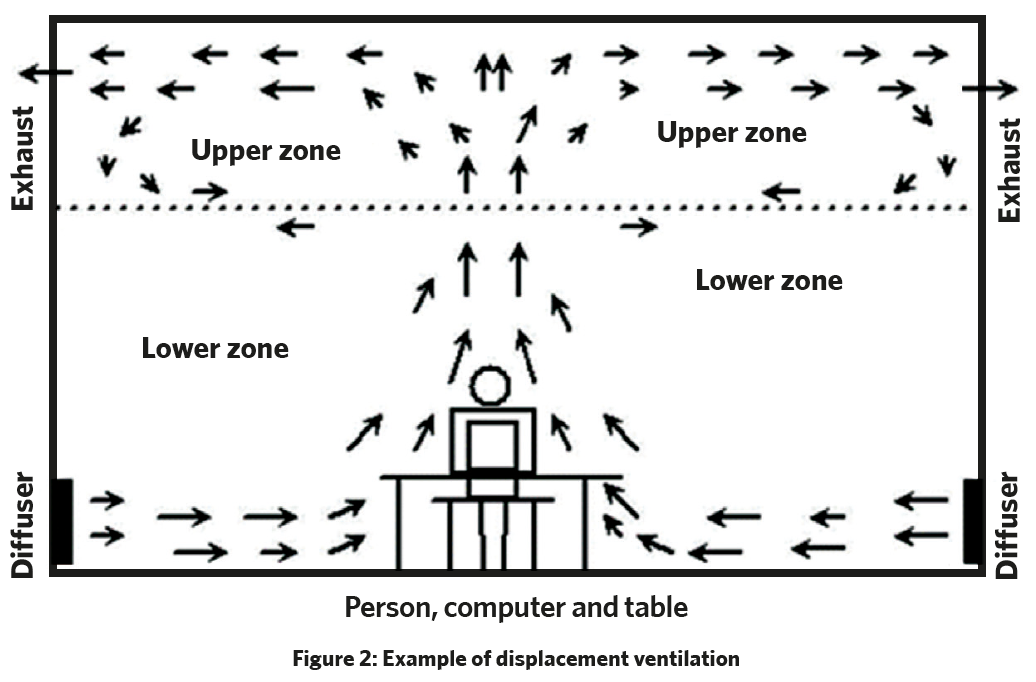
In 2011, two further papers were published, collating performance data for mechanical, natural and hybrid ventilation systems and attempting to quantify the difference between displacement and mixing ventilation with regards to effectiveness at removing pathogens. Amir Aliabadi et al concluded that a vertical, upward-type displacement ventilation that introduces fresh, cool air near the bottom of the room is far superior to top-down mixing ventilation, as the buoyant force takes the warm and polluted air (possibly containing airborne pathogens) close to the ceiling and subsequently the exhaust for removal.8
Yonggao Yin et al managed to conduct comparative tests (again, in a hospital ward) and arrive at a numerical evaluation: 4ACHD > 6ACHM (displacement ventilation with 4ACH removed tracer gas and fine aerosols much more effectively than the mixing type ventilation with 6ACH).9 If any exhaust was located at low level, (ventilation flow against buoyancy) the pollutant concentration at breathing zone would be even worse than when using a mixing type of ventilation. The paper concluded that for the best result for pathogen removal, all exhausts must be located at high levels, preferably closer to the pollutant source with fresh air delivered low.
Back to the present
Several studies published in 2020 and 2021 arrived at similar conclusions. One focused specifically on the mixing ventilation in hospitals and established that even at 12ACH (equivalent to 120L.s-1 per person) the top-down mixing ventilation failed to remove virus pathogens from two-person wards.10
A team at the University of Cambridge found that mixing ventilation systems disperse airborne contaminants evenly throughout the space. These contaminants may include droplets and aerosols, potentially containing viruses.
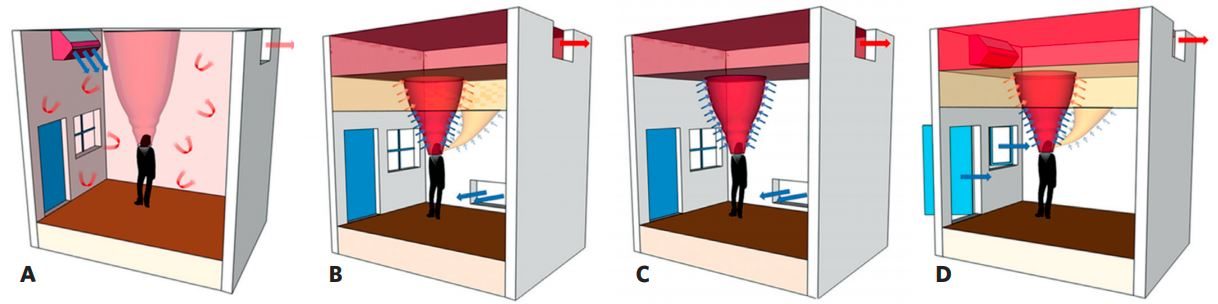
Figure 3: Illustration of ventilation flows with the various flow elements such as the body plume, exhaled breath, inlet flows, stratification and arrows indicating entrainment and mixing
The conclusion was that displacement ventilation, which encourages vertical stratification and is designed to remove the polluted warm air near the ceiling, is the most effective at reducing the exposure risk.11
A University of Oregon study concluded that recirculating or mixing airflow has the potential for high spread of coronavirus-infected droplets within densely occupied spaces, even with just one person exhaling the virus droplets. Apart from the recirculation, transmission appears to be facilitated by the type and velocity of turbulent airflow designed to reach deep into the occupied space.12
Conclusion
We need to take a closer look at how we ventilate buildings, especially with high occupancy. Thinking just in terms of ACH is way too simplistic. We spent the past few decades sealing office windows and fitting positive pressure, mixing ventilation into ceiling voids – I believe we were going in the wrong direction.
The question is how can we adapt existing buildings to a Covid-conscious future? Not every building can be naturally ventilated – although, surprisingly, many can – and not every HVAC or every space can be easily converted to displacement ventilation (supplying air slowly at low level and extracting at high level).
Those hard-to-adapt spaces may need to transition to lower occupancy levels or to more individual setups (less open plan) accommodating more flexible working arrangements. This means that working from home might not always lead to a reduction in office space requirement – and lower estate costs.
About the author
Tom Lipinski is founder and technical director at Ventive
References:
- Exaggerated risk of transmission of COVID-19 by fomites, The Lancet
- How the world missed Covid-19’s silent spread, The New York Times
- 239 experts with one big claim: the coronavirus is airborne, The New York Times
- Roadmap to improve and ensure good indoor ventilation in the context of COVID-19, WHO,
- SL Miller, WW Nazaroff, JL Jimenez, A Boerstra, G Buonanno, S J Dancer, J Kurnitski, LC Marr, L Morawska, C Noakes, 2020. Transmission of SARS-CoV-2 by inhalation of respiratory aerosol in the Skagit Valley Chorale superspreading event, International Journal of Indoor Environment and Health, 314-323.
- Birnir, Björn, 2021. Ventilation and the SARS-CoV-2 Coronavirus Analysis of outbreaks in a restaurant and on a bus in China, and at a Call Center in South Korea
- Hua Qian, Yuguo Li, WH Seto, Patricia Ching, WH Ching, HQ Sun, 2010. Natural ventilation for reducing airborne infection in hospitals, Building and Environment Volume 45, Issue 3 559-565.
- Aliabadi, Amir, A & Rogak, Steven & Bartlett, Karen & Green, Sheldon, 2011. Preventing Airborne Disease Transmission: Review of Methods for Ventilation Design in Health Care Facilities. Advances in preventive medicine 124064. 10.4061/2011/124064.
- Y Yin, W Xu, JK Gupta, A Guity, P Marmion, A Manning, B Gulick, X Zhang & Q Chen, 2011. Experimental Study on Displacement and Mixing Ventilation Systems for a Patient Ward. HVAC&R Research
1175-1191. - Juan Ren, Yue Wang, Qibo Liu, Yu Liu, 2021. Numerical Study of Three Ventilation Strategies in a prefabricated COVID-19 inpatient ward. Building and Environment 188 (2021) 107467.
- RK Bhagat, MSD Wykes, SB Dalziel, PF Linden, 2020. Effects of ventilation on the indoor spread of COVID-19. Journal of Fluid Mechanics Volume 903.
- Leslie Dietz, Patrick F Horve, David A Coil, Mark Fretz, Jonathan A Eisen, Kevin Van Den Wymelenberg, 2020. 2019 Novel Coronavirus (Covid-19) Pandemic: Built Environment Considerations To Reduce Transmission. Applied and Environmental Science.
- RK Bhagat, MSD Wykes, SB Dalziel, PF Linden, 2020. Effects of ventilation on the indoor spread of COVID-19. Journal of Fluid Mechanics Volume 903.