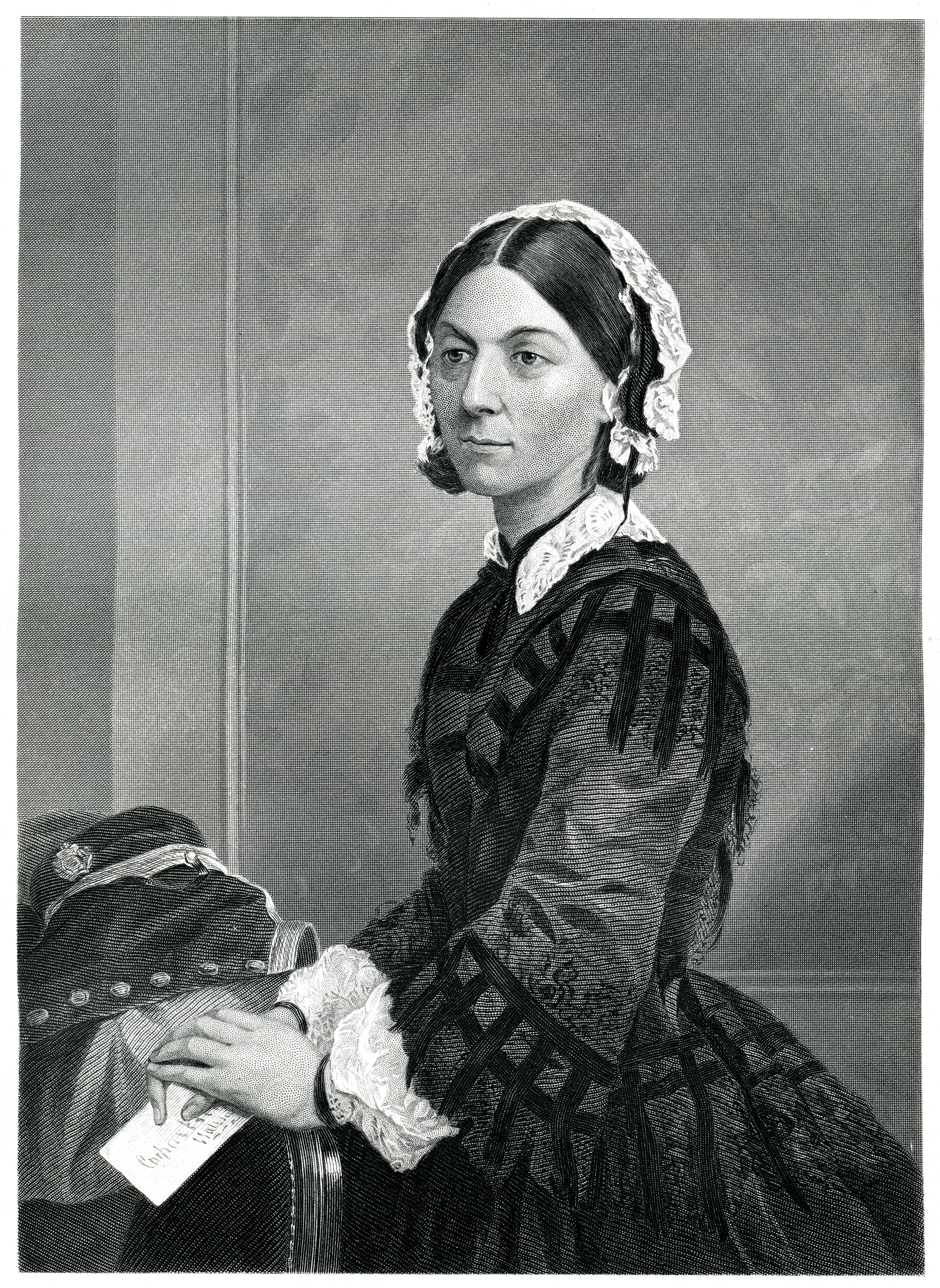
The 200th anniversary of the birth of Florence Nightingale takes place this month and it is testament to her legacy that she remains a symbolic characterisation of the nursing profession, with the recent opening of NHS Nightingale Hospitals in the UK.
She is credited with being the founder of modern nursing, but less well known is her work on ventilation and hospital design – and it is perhaps apt that, in these challenging times, the rapidly completed hospital is named in her honour (see also Florence Nightingale: nurse and building engineer, CIBSE Journal, June 2015).
It is worth contemplating why Nightingale’s work on ventilation is less celebrated when the opening chapter of her seminal book, Notes on Nursing – first published in 1859 – focuses not on patient care, but on ventilation.1 She writes: ‘The very first canon of nursing… keep the air he breathes as pure as the external air, without chilling him.’
Nightingale continually emphasises the importance of ventilation in ensuring the swift recovery of patients and reducing cross-infection. She had considerable first-hand experience of the reduction in infection rates and health benefits provided by improved ventilation. This was at a time when germ theory was not well established; in the mid-19th century, it was acknowledged that – as well as expelling exhaled carbon dioxide – other unhealthy organic miasmas should be removed as quickly as possible.
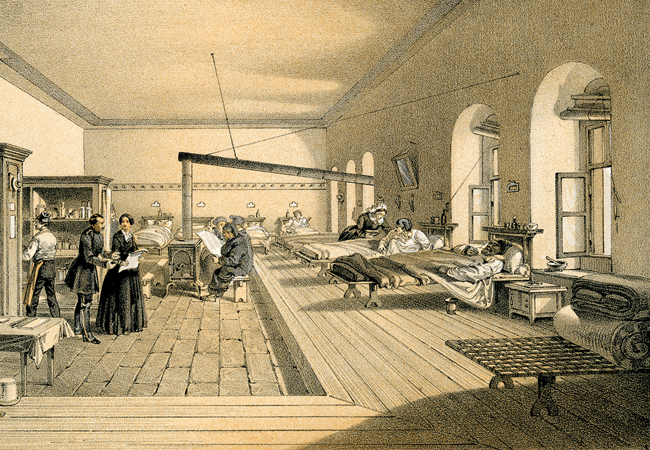
Nightingale wasn’t the first to identify the importance of ventilation in hospitals. Her conclusions in Notes on Nursing were the culmination of 15 years’ work initiated by David Boswell Reid. His comprehensive ventilation systems were devised for hospitals in London, Copenhagen, Chicago and New York, long before the Crimean War (1853-1856) thrust Nightingale into the spotlight. However, she used her high profile to promote the need for ventilated wards.
There is important crossover in these times of a pandemic. Ventilation and air quality have not received the kind of exposure in the popular press as energy efficiency in recent years, yet it remains fundamental to the delivery of good indoor health and wellbeing.
Nightingale’s experience during the Crimean War of dealing with cross-infection – which was responsible for 80% of deaths – TB and other infective diseases would, I am sure, focus her attention on the ventilation design of all newly built wards. Without the kind of understanding of microbes and viruses that we have today, it was evident to her that ventilation was a primary solution to reduce cross-infection.
The primary means of transmission of the SARS-CoV-2 virus is believed to be through contact with contaminated surfaces or by large virus-laden droplets emitted by infected individuals. However, work undertaken on viral transmission over the past few decades, especially in the wake of the Sars epidemic in 2002-04, has looked at the role of virus-containing aerosols that may become entrained in air plumes and remain airborne for several hours, travelling much further than the 2m social-distancing requirement.
Nightingale had experience of the reduction in infection rates and health benefits provided by improved ventilation
Bourouiba and Asadi postulate that such aereolisation could well be a route of transmission of SARS-CoV-2,2, 3 although it is important to understand that the further away from the source, the more diluted the virus will become.
Linsey Marr, a professor at Virginia Tech with expertise in airborne transmission of infective diseases, outlined in a recent tweet thread the implication of what this may mean.
At close range (imagine a plume of cigarette smoke), the concentration of airborne virus will be quite high. As you get further from the source, the concentration falls off rapidly. If you are close, you are much more likely to inhale the virus. You are also more likely to be sprayed by large droplets that land on your face, which doesn’t happen if you’re further away.
Viruses in small droplets can float around in air for many hours, but they will probably be quite diluted unless you’re in a small confined space. You could inhale these, but it’s much less likely than if you’re close to the person.4
The key here, with respect to ventilation design, is the reference to a small confined space. Risk of infection is exposure × time, so it stands to reason that, in a poorly ventilated space, there is an increased risk of exposure time to virus-laden aerosols that are not being diluted sufficiently.
It is important to note that, because SARS-CoV-2 is a novel virus, there is little empirical proof that transmission can occur by exposure to such aerosols, with some circumstantial evidence beginning to emerge. 5,6,7,8,9 Nevertheless, we do have evidence that Sars and other viral infections do transmit via this route.
Nightingale did not understand fully about germ theory when promoting good ventilation design. Likewise, even if we do not know definitively that SARS-CoV-2 may transmit in this way, it is important that we, as building service engineers, give appropriate consideration to buildings being repurposed to house Covid-19 patients, to ensure ventilation solutions provide the maximum dilution possible, to help reduce infection risks.
We know that ventilation in some buildings is less than adequate, especially where occupants do not fully understand the principles of the ventilation design . So we should, where possible, remind building occupants to open vents and windows (taking care not to compromise pressure isolation areas) to ensure adequate ventilation and, in mechanical systems, turn off recirculation in HVAC, and increase ventilation rates where possible. It may just help reduce infection risk by ensuring adequate dilution of any airborne viral presence.
References:
1 F Nightingale, Notes on nursing: what it is, and what it is not, Harrison London, 1860
2 L Bourouiba, Turbulent gas clouds and respiratory pathogen emissions – potential implications for reducing transmission of Covid-19, JAMA. Published online 26 March 2020. doi:10.1001/jama.2020.4756
3 Sima Asadi, Nicole Bouvier, Anthony S Wexler and William D. Ristenpart (2020), The coronavirus pandemic and aerosols: does Covid-19 transmit via expiratory particles?, Aerosol Science and Technology, doi: 10.1080/02786826.2020.1749229
4 L Marr, Twitter, April 2020
5 J Lu , J Gu, K Li, C Xu, W Su, Z Lai et al (2020), Covid-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020, Emerging Infectious Diseases.
6 N Van Doremalen et al (2020), Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1, New England Journal of Medicine. doi 10.1056/NEJMc2004973
7 H V Fineberg, Rapid expert consultation on the possibility of bioaerosol spread of SARS-CoV-2 for the Covid-19 pandemic (1 April 2020).
8 Guo Z-D, Wang Z-Y, Zhang S-F, Li X, Li L, Li C, et al. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg Infect Dis. 2020 Jul [13-04-2020]
9 Lidia Morawska, Junji Cao, Airborne transmission of SARS-CoV-2: The world should face the reality, Environment International, Volume 139,2020,105730






