Using an existing building is one of the fastest and safest ways of implementing temporary medical facilities, says Arup
In the UK, the rapid conversion of conference centres into emergency Nightingale Hospitals – such as at the ExCeL in London – was one of the most visible healthcare infrastructure responses to the initial threat of hospital capacity being overwhelmed by a surge in Covid-19 patients. And now the ‘second wave’ of the pandemic in the UK is upon us, some of these facilities are back on standby.
While these emergency field hospitals were designed to address potentially critical shortages of ICU and ward beds at short notice, other projects have been under development that provide alternative models for temporary healthcare facilities. These are informed by incorporating the increasing knowledge of how the SARS-CoV-2 virus spreads into their building design principles.
Two alternative design responses for temporary hospitals include the CareBox modular hospital system developed by Arup and, from University of Cambridge Professors Andrew Woods and Alan Short, a series of practical solutions to reduce the concentration of airborne virus experienced by patients and healthcare workers in buildings converted into makeshift emergency Covid-19 wards.
CareBox
CareBox has been developed by Arup as a series of design guidelines for scalable, modular solutions that can be deployed quickly in a range of settings to add emergency hospital capacity. It is designed to offer flexibility to expand critical care or ward capacity either at existing hospital campuses or through the conversion of existing facilities, such as multi-storey car parks or conference facilities.
The modular solution was developed to be applicable to a number of different contexts as well as spaces, so that it could be deployed in a variety of national healthcare systems – ranging from well-resourced European or American-type scenarios to low-resource base healthcare environments, such as in developing countries. A current example of the latter is Arup’s work with NGOs at refugee camps at Cox’s Bazar in Bangladesh.
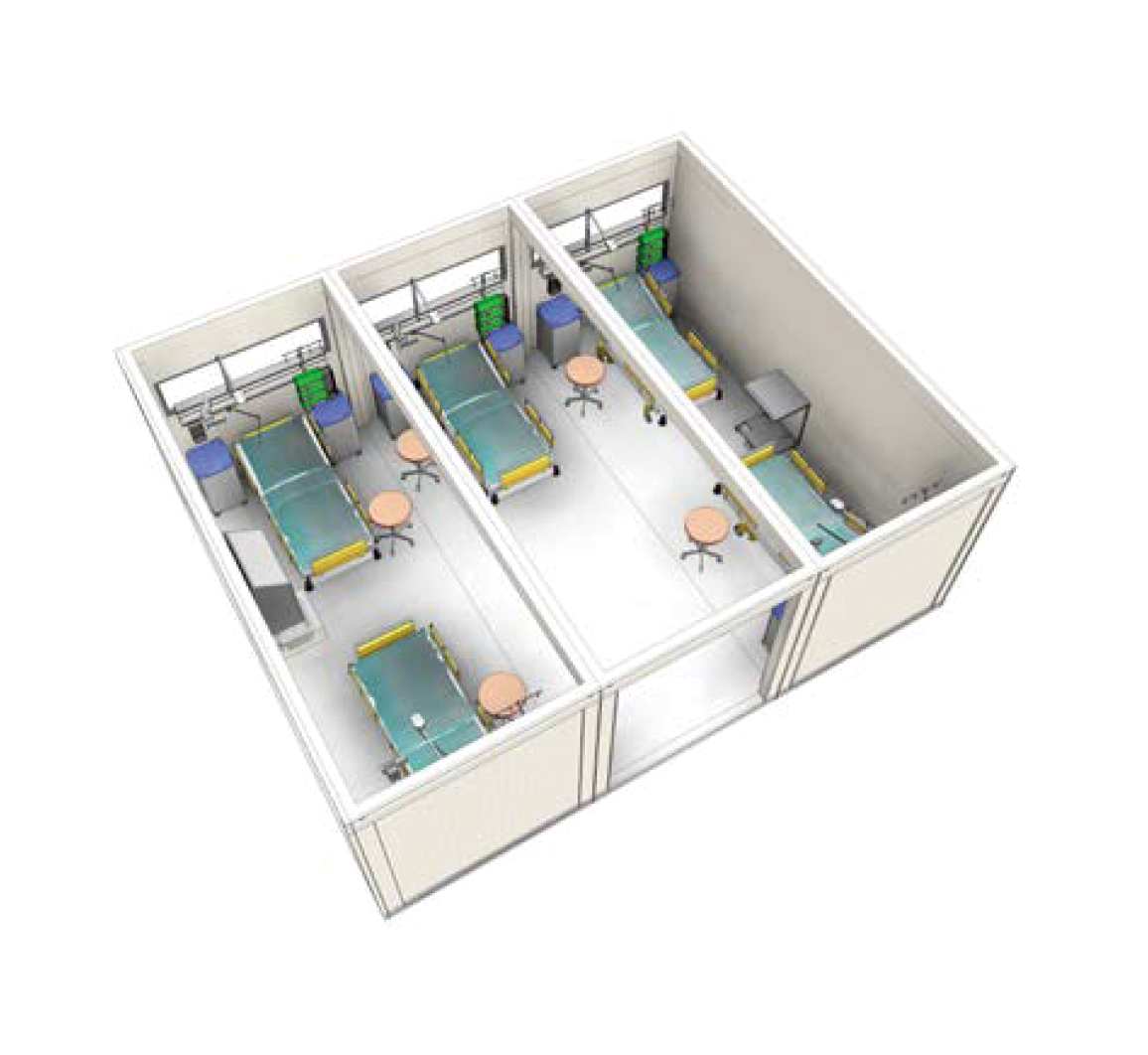
Ward module: Three modules become an independent box of five oxygen-assisted beds
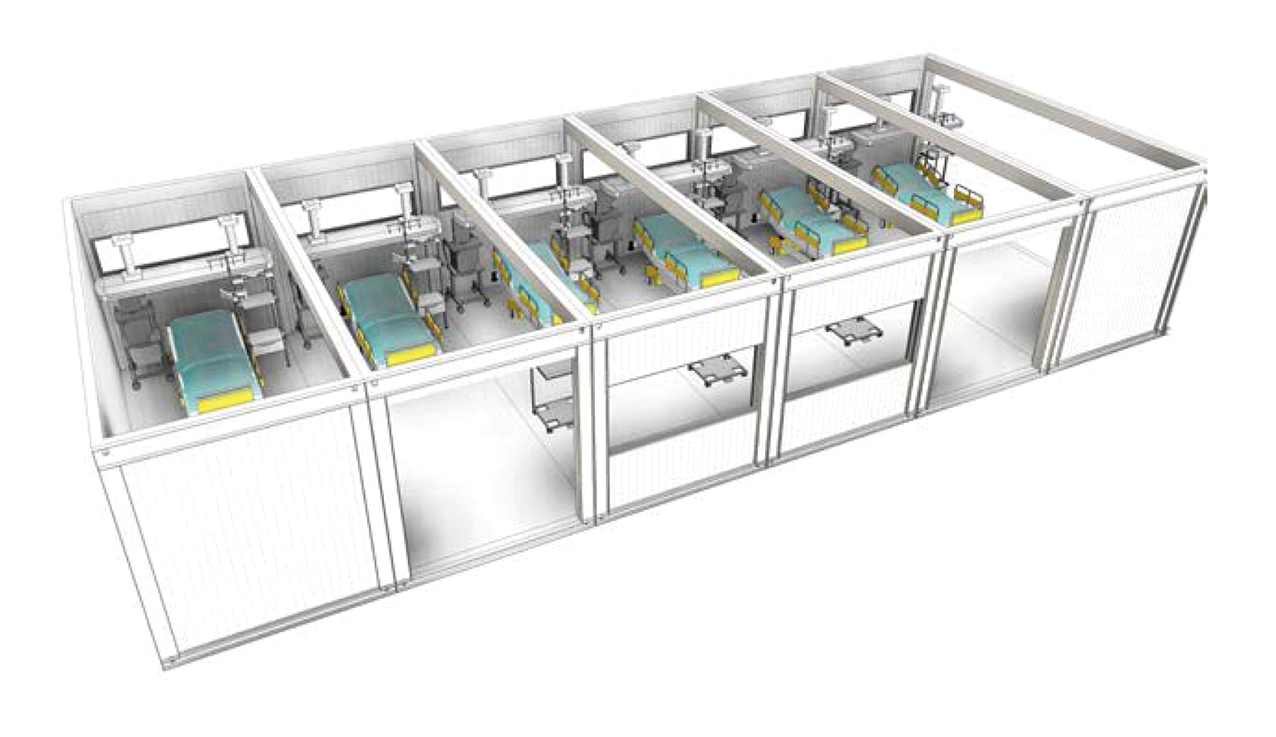
ICU module: Six-to-12 modules become a long box of six-to-12 ICU beds

Support modules: The central spine allocates modules for different uses: pharmacy, resting area, WCs clean/dirty utility, storage, and so on
To cater for these different scenarios, the CareBox design guidelines have evolved into four variants, which are free to download from Arup’s corporate website. These include a ‘plug-in’ design for adding extra space to an existing hospital facility; a ‘multi-storey’ solution for expanding capacity in confined spaces, such as car parks next to hospitals; an ‘in-door’ design for adapting existing buildings such as convention centres or sports halls; and a ‘low-resource’ model for regions with more limited healthcare facilities. Each contains specifications for building and fitting out the CareBox, with detailed design of building services and processes necessary to create a fully functioning emergency healthcare facility.
‘The reference points we used in the design development were from our existing healthcare project portfolio,’ says Dan Moran, associate director at Arup’s buildings team in Dublin, Ireland. ‘We incorporated sound engineering principles aligned with World Health Organization (WHO) guidance, and then cross-referencing that back to Health Technical Memoranda (HTM) recommendations, to make sure we were putting together a robust solution.’
Moran, who has been working in Arup’s healthcare business for 12 years, says the initial concept was the result of a collaboration with an architect through Arup’s Madrid office. It was initially based around the idea of a shipping container-type solution adapted for medical requirements, although this quickly evolved.
‘As it developed, we recognised that our multi-disciplinary team could bring further refinement across the design,’ says Moran. ‘We engaged across our team including engineering designers, fire consultants, manufacturing and logistics to understand the various challenges and how we could respond. We also had great engagement with industry as firms sought to assist in the development of solutions.
‘We also carried out CFD analysis for particular areas, such as ICU, to examine the airflows in the spaces created, thereby identifying any areas that may have low air movements. This informed the detailed design of the spaces and identified the need for supplementary shunt fans or ventilation. We were also keen to maximise the use of cascading air pressures in the different clinical spaces to control the potential spread of the virus. This provides a safer environment for both clinical staff and patients, whereby more infectious patients are kept in lower relative pressure spaces, with passive airflows or dedicated air-curtains providing a barrier to transmission.’
This approach reflects the developing WHO understanding of the virus transmission.
CareBox designs can evolve as understanding of potential airborne transmission of the virus increases
Modular solution
The adaptability and modularity of the design is intended to facilitate rapid deployment and flexibility, explains Moran. ‘The idea behind CareBox is that you could develop this in a factory, ship it to wherever it’s needed, fit it out and it’s ready to go. Full fitout of the spaces, including equipping, can be done in a factory setting, with local tie-ins and integration completed on site. You can design the solution off site and bring it on site and implement it very quickly.’
Moran says the design can be used for ICU or regular wards as required, with appropriate services added according to whether local infrastructure – such as power or liquid oxygen VIEs – are available to be connected from an existing healthcare site or have to be supplied as part of a modular bolt on.
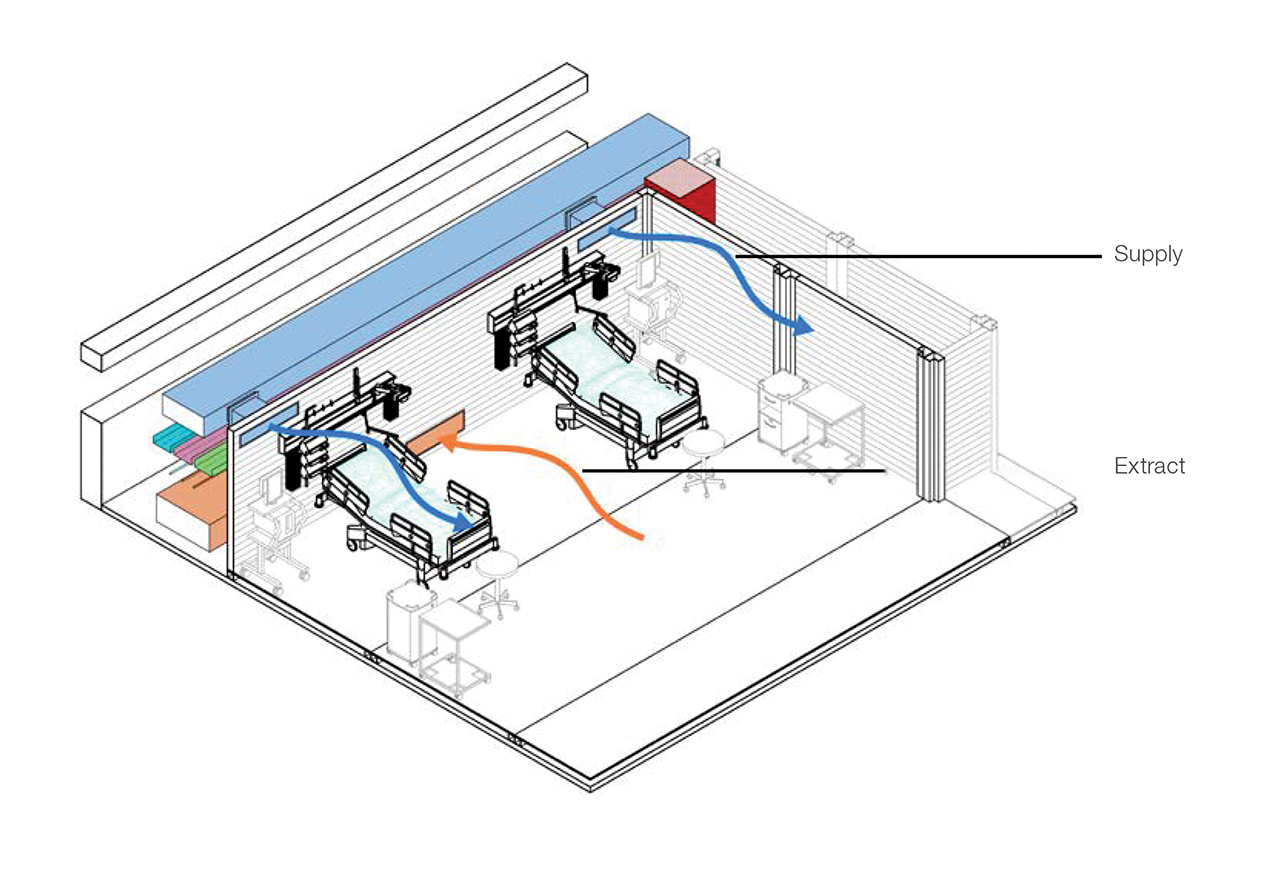
Air will be supplied at high level and extracted at low level in multistorey facilities
‘It also means that when the facilities are no longer needed, they can be taken apart and redeployed elsewhere or put into storage. Or it could be used as a legacy project for the community, particularly in lower-resource type situations or countries where the healthcare system may be short of beds.’
Moran says the CareBox designs are adaptable enough to evolve as understanding of potential airborne transmission of the virus increases. ‘With CFD analysis and modelling, you can see where the airflow is going within spaces, and where you may have a concentration of pathogen because of poor airflow. Once you have that level of understanding, you can design low-tech solutions to help airflow, such as shunt fans or more ventilation. We’re starting to look at the interactions for CareBox to introduce a little more sophistication into what that analysis might be, and how it could work.’
Responses
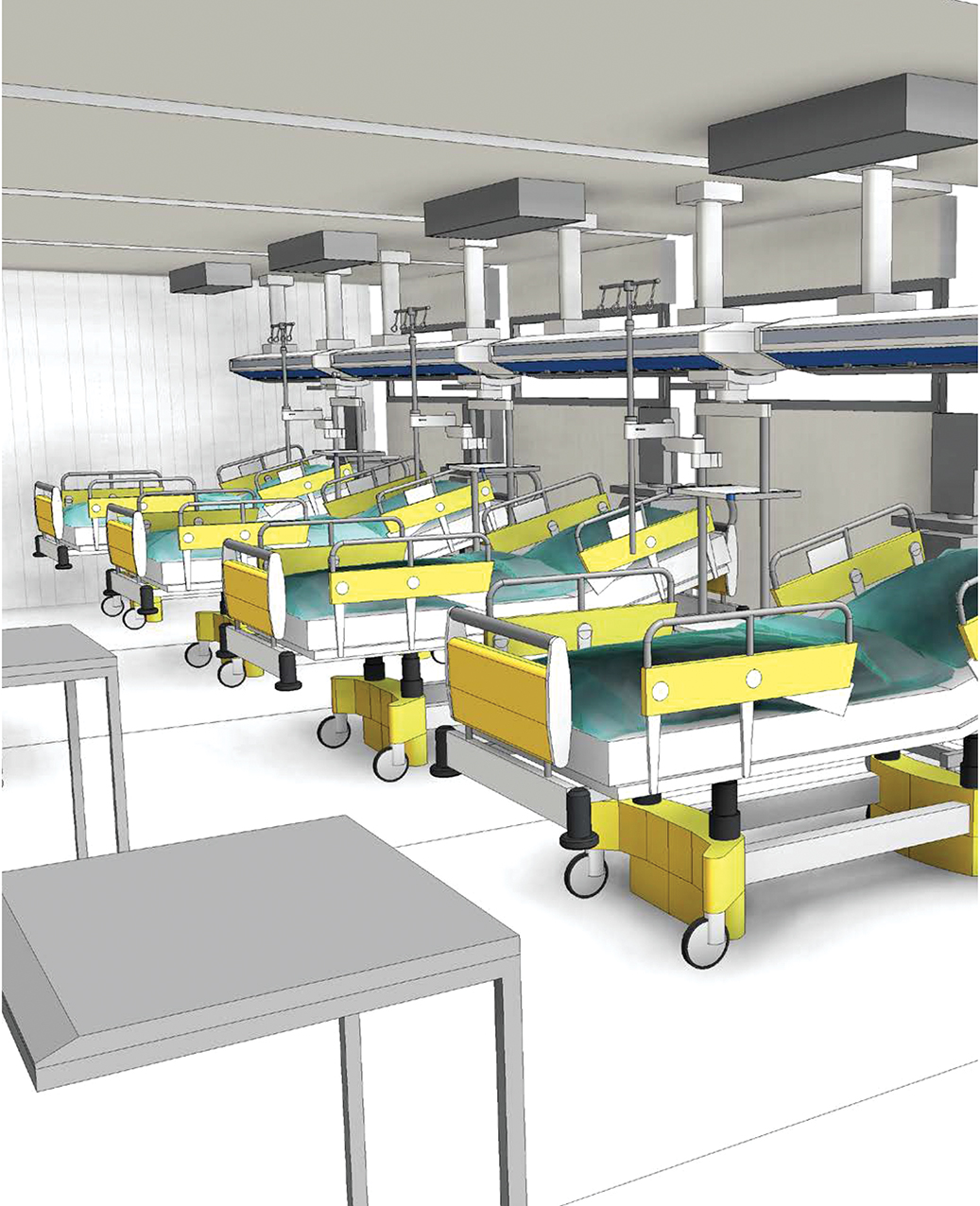
Each ward module can accommodate five moderate or severe Covid-19 patients
As healthcare organisations cope with the second wave of Covid-19, the demand for CareBox-type solutions may depend on the type of responses authorities take and whether smaller, more localised solutions, rather than large-scale Nightingale-type facilities, may be necessary.
Although it has yet to be deployed in its modular form, Moran says Arup has been in discussions about possible adoption of CareBox solutions with several NHS healthcare trusts in the UK and various healthcare organisations in South America.
He says: ‘The Nightingale Hospital-type solutions provided effective surge capacity as the starting point. However, health authorities are now looking for more resilient solutions to enable them to deal with Covid patients, while maintaining care and treatment of other patient cohorts. This is particular evident as health authorities assess the likely impacts of the next wave of Covid-19.’
Arup has taken an open-source approach to CareBox and is sharing the guidelines freely so facilities can be implemented across communities when they are needed.
University challenges
Two University of Cambridge academics have developed a series of low-tech ventilation and ward configuration solutions that they claim can significantly reduce the dispersal of airborne virus in buildings that have been converted into emergency Covid-19 healthcare facilities.
Professor Andrew Woods, of Cambridge’s BP Institute, and Professor Alan Short, of the Department of Architecture, say the type of large air-conditioned halls that have been rapidly converted into emergency hospital facilities tend to feature top-down air conditioning, which creates turbulent flows that can mix and spread droplets containing the virus very widely.
Their research (shown in a video report) suggests that, with six changes of the air in the occupied part of the hall in an hour, it may take more than 20 minutes to dilute the concentration of smaller droplets produced in a cough to below a tenth of their original density. This creates a hazardous environment for healthcare workers as they pass through ‘a slowly refreshing miasma’.
‘Effective ventilation is critically important in helping to suppress cross-infection, and nowhere more so than in an infectious diseases ward,’ explains Short, adding: ‘Our research shows that a small number of straightforward modifications would reduce risk in what is already a very risky environment.’
The Cambridge team’s recommendations are based on physical laboratory experiments to test ventilation systems for two basic bed arrangements: a typical open hall with hundreds of beds with low-level partitions; and with beds arranged within enclosed patient bays, partitioned at the side and sealed above (such as with polythene) so that, as far as possible, the exhaust air does not permeate the rest of the hall.
In the open-hall scenario, the movement of the ventilation air means that, when a patient coughs or releases aerosols, the flow pattern of the aerosols can extend across the space to other patient beds.
In the enclosed patient bays with exhaust ducts located behind the patients’ beds, aerosols from coughs potentially spreading the virus are contained within the space, and the high levels of aerosols retained there are rapidly removed by the ducts, minimising the spread of virus into the main ward space.
The services configuration proposed by the Cambridge team sees contaminated air drawn from the exhaust ducts collected in ‘dirty corridors’ running laterally across the facility before being discharged from the building. In this way, the spread of the virus can be minimised in the main areas between bays and ‘clean’ corridor spaces that healthcare workers can use within the facility.
The solution has been designed to be suitable for a variety of climates and the Cambridge team is currently working with Professor LS Shashidhara from Ashoka University, an adviser to the Indian government, and architect CS Raghuram, to create viable conversions of marriage halls and sheds as emergency Covid-19 hospitals in India.