With the emergence of Covid-19 – a virus spread by aerosols – there has been growing interest in the use of ultraviolet (UV) light to disinfect air in buildings.
Ultraviolet germicidal irradiation (UVGI) is a disinfection method that uses short-wavelength ultraviolet C (UV-C) light to kill or inactivate microorganisms by destroying nucleic acids and disrupting their DNA and RNA.
Although not a new technology, having been pioneered in 1930s America by William F Wells to reduce the transmission of measles among schoolchildren, Covid-19 has sparked renewed interest in UVGI as a possible countermeasure to the virus.
Upper-room installations rely on natural convection currents to carry aerosol particles through the UV field, and can be particularly effective, often achieving very high equivalent air-change rates
Researchers from industry and academia have found evidence that suggests SARS-CoV-2, when suspended in air, is reasonably easy to inactivate using UV light at 254nm.
Clive Beggs, emeritus professor at Leeds Beckett University, has been researching UV air disinfection to reduce Covid-19 transmission in buildings, and his research paper has recently been published by PeerJ, the biological, medical and environmental sciences journal.
The question, he says, is not whether UV works – we know it does – but whether we ‘can deliver the dose that’s necessary to prevent the transmission of infection?’ When considering UVGI air disinfection, he adds, it is important to evaluate its likely performance in the context of the space, which will depend on occupancy levels, room geometry and the ventilation system.
UVGI devices can be divided into three main application classifications: upper-room, in-duct, and room air cleaners. All have benefits, but there is a distinct lack of guidelines for their design and installation, says Beggs. There is also a need for manufacturers to undertake robust microbiological testing and fully characterise the UV fields (UV light beam produced by the lamps) created by their devices.
UVGI room air cleaners
These standalone devices are located within a room and use UV-C lamps mounted in a container with a fan. Air enters the device and is drawn by the fan over a UV lamp before being blown back out into the space, says Beggs, who was a HVAC design engineer before specialising in air disinfection and the transmission of diseases in hospitals.
Although room air cleaners are efficient at disinfecting the air that enters the device, they are only as good as the fan. ‘If you’ve got a small device with a small fan, all the air that passes over the UV lamp might be cleaned and disinfected, but not much air is going through,’ says Beggs, who adds that many manufacturers claim such units achieve a 99.9% disinfection rate.
Calculating the right UV flux will depend on the room geometry and lamp geometry, as well as the room airflows, so good software will be key
‘This is true, but these claims only relate to the air that passes through the UV device, and not the effect the unit will have on the room space. If you’ve got a very big room and a small device, you’re not going to get much impact.’
Nathan Wood, managing director at ventilation firm Farmwood M&E, and chair of BESA’s Health & Wellbeing in Buildings Group, says UVGI room air cleaners are most effective in contained spaces, including non-ventilated meeting rooms or classrooms, used by a lot of people sequentially.
He has been installing UVGI Radic8 Virus Killer units for several years. The freestanding or wall-mounted devices use technology, developed with the South Korean government in response to the SARS outbreak in 2003. They comprise course, Hepa and carbon air filters and multiple UV tubes, each surrounded by a reactor chamber that reflects and refracts the light, magnifying the reaction. Wood says a unit can process up to 18 cubic metres of air per minute, eliminating 99.9999% of pathogens – known as a Log 6 reduction.
Since lockdown in March, the two MVHR systems at Farmwood’s office have been recommissioned to supply more outside air, while its UVGI systems have been repositioned to ensure the best airflow, following the office’s new socially distanced layout. ‘The grill configuration needed to be changed as the high-level acrylic screens reduced the airflow in the room,’ says Wood. ‘We plan on further revamping the ducting layout to allow for high-level supply and low-level extract. With additional UVGI units on desks we’re able to zone each working area and reduce the risk of any potential aerosolised particles leaving it.’
When installing such units, design engineers must do their research on suppliers, adds Wood. ‘They should have independent testing from specialised labs, history of real life application and results, and time served experience with the technology,’ he says.

JenAct’s UV Torpedo
In-duct UVGI
These systems use UV-C lamps mounted in return or supply air ducts of mechanical HVAC systems, to disinfect air to or from the room space. In the US, UV-C lamps have been installed in return-air ductwork to mitigate the spread of tuberculosis. As Covid-19 is also a disease spread by aerosols, this system would, in theory, be equally applicable to the coronavirus, says Beggs.
Infectious droplets, which start at 100 microns (μm), evaporate down to less than 50μm diameter rapidly, so they can float around in air currents and get taken into return air ducts. ‘Central HVAC systems can recirculate as much as 50-80% of the room air during the winter, so the virus on aerosol particles could be drawn up into the return air duct and recirculated round, potentially resulting in the spread of Covid-19,’ says Beggs.
A possible retrofit solution, he suggests, might be to put UV lamps in the return air duct, disinfecting the air before it passes filters and coils. This way, not only is the recirculated air disinfected, but the maintenance staff are also protected from contamination – and the exhaust air is cleaned.
It’s easy to retrofit such devices into ducts, says Beggs. However, if the air velocities are too high – or the lamps are too weak – the aerosol particles carrying the virus may not be irradiated for long enough to inactivate them, which is a potential problem.
‘If you have big ducts and fast-moving air, you may have to have huge lamps – which means you’ll have electrical loads of several kilowatts,’ he says. ‘This can be a substantial additional load in some buildings.’
Design is another issue, as manufacturers can place lamps in different geometrical arrangements. As a result, sophisticated modelling technology – such as computational fluid dynamics – is needed to calculate the UV field required for a particular duct size, air velocity and lamp arrangement.
UVGI systems manufacturer JenAct, part of Jenton Group, uses a radiation (light distribution) model to calculate the UV dose needed to achieve full log disinfection, based on the airflow, duct size and target virus.
Dr Jarek Bilek, a director at JenAct, who developed the software, says: ‘Based on the dispersion of radiation within a space, we can calculate the dose – or energy – that the virus is exposed to on the way through the duct.’
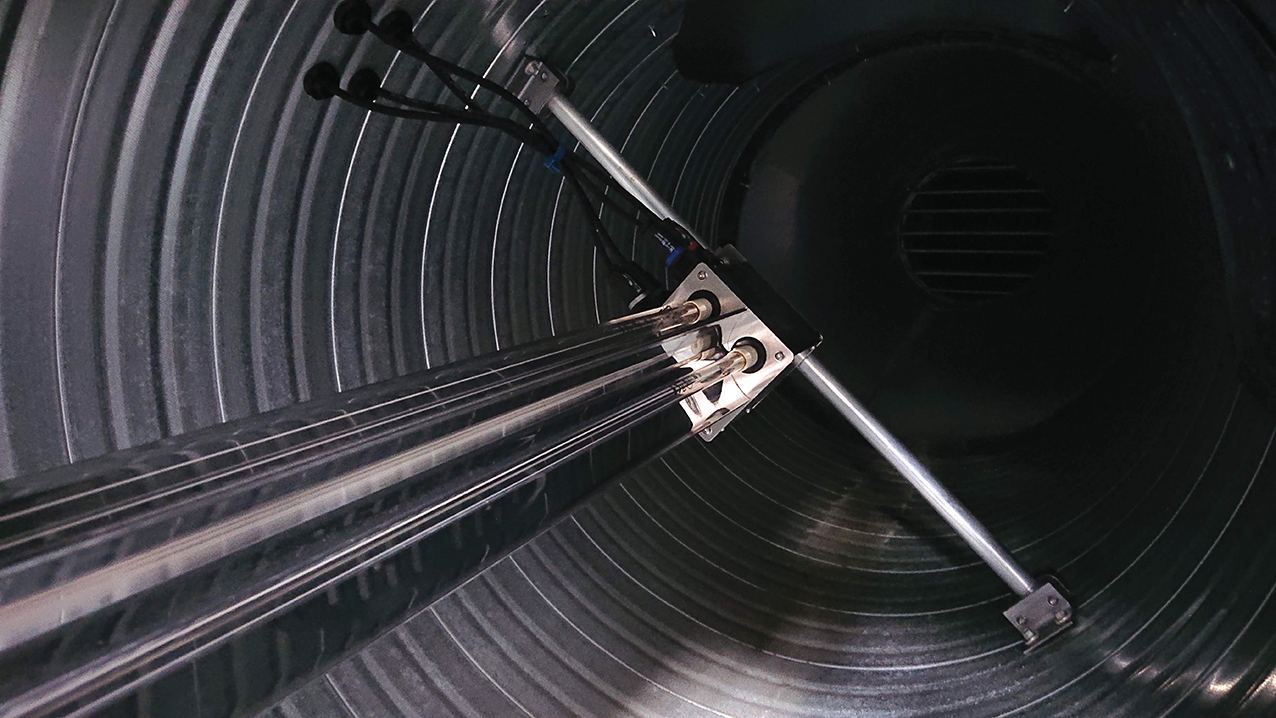
JenAct’s UV Torpedo installed in a duct
The firm’s UV Torpedo in-duct unit, mounted longitudinally in the middle of a return- or supply-air duct, has been installed in a UK food factory recently. However, uptake of the technology has mostly been in the US and the Middle East, where air conditioning, heating and cooling is prolific in buildings, says Richard Little, another director at JenAct.
Little believes evidence of the effectiveness of UVGI in disinfecting aerosols has been slow to come through because, unlike with bacteria, carrying out scientific studies on the virus requires certified laboratories. ‘Recent work by Boston University has confirmed UV-C doses required to disinfect SARS-CoV-2,’ he says. ‘It has been established that SARS-CoV-2 needs far less energy for disinfection than moulds and bacteria, so there is supporting evidence that the UV-C systems will be effective, and we can feed that data into mathematical models to get appropriate specifications.’
Bilek adds: ‘One of the features of UV is that it’s so versatile – it can be fitted into any size duct and matched to any airflow – but all the possible variations have not been tested.
‘Because of the variety of ducts and airflows, various air temperatures and humidity, to ask for proof for every application with different parameters is a big hurdle for the introduction of these products into the market.’
Upper-room UVGI
These systems create an open UV-C irradiation field above occupants’ heads to disinfect aerosolised bacteria and viruses suspended in the air.
Upper-room installations rely on natural convection currents to carry aerosol particles through the UV field, says Beggs, and can be particularly effective, often achieving very high equivalent air-change rates. ‘Potentially, they should be very effective against Covid-19’, he adds. However, as Covid-19 is transmitted by larger aerosol particles – some of which can fall out of the air – it is important that the air is well mixed, and this may require the system to be supplemented with extra room fans.
Calculating the right UV flux will depend on the room geometry and lamp geometry, as well as the room airflows, so good software will be key. ‘This is a hugely important retrofit technology – I can see it being very useful in lecture theatres, pubs, restaurants, nightclubs, theatres, concert halls, schools – wherever lots of people congregate and the risk of Covid-19 transmission is high,’ says Beggs.
Despite the great potential of this, Beggs adds that there appears to be little interest on the commercial side in the UK for upper-room UV, with most applications in the US.
Key questions that engineers should ask
Professor Clive Beggs says the first thing to look for on a manufacturer’s website is scientific evidence, for a measure of how much knowledge they have. ‘Have they done any microbiological testing? If they have results, this shows they are a company that has put some investment into this.’
If it’s an in-duct UV system, ask for supporting calculations of the dose that the average particle is going to get, he adds. ‘I would expect a manufacturer to be able to produce robust calculations for the UV field they are proposing to use, so that it meets your specification.’
Redundancy is an issue too, so it is also important to ask what would happen if a lamp goes out.
Need for guidelines
Given the complexity of designing UVGI air disinfection systems, the lack of guidelines in the industry is perhaps not surprising.
‘Guidelines are needed to ensure installers are confident to use UV, and to tell design engineers what to ask for,’ says Bilek. ‘But, rather than suppliers, the guidelines should come from an association, the government or another authority that industry professionals trust. We are sharing our data with a couple of associations trying to do just that.’
It is also worth remembering the limitations of the technology, says Beggs. ‘While UVGI air disinfection can help reduce aerosol transmission, it cannot protect against close-range droplet transmission.’
So, measures such as wearing face coverings, social distancing, not mixing so much and washing our hands will need to continue to be applied. ‘We want the economy to work and venues need to be operational, so I can see great potential for these types of UVGI technologies. They will not prevent the disease completely, but they will help mitigate the spread,’ Beggs says.
‘Another pandemic will come along in time, so – if we’re serious about mitigating diseases caused by aerosols –this technology is important.’
