The control of the legionella bacteria and avoiding the risk of incidents of Legionnaires’ disease (and Pontiac fever) are justifiably regarded as essential for both the products and the systems designed for the servicing of buildings. The impact of poorly designed or operated hot water distribution systems poses a significant risk.
More than 50 species of legionella have been identified1, and half of these can cause infection that may be either asymptomatic or result in one of the forms of legionellosis. However, practically all of the cases of infection reported throughout Europe are caused by legionella pneumophila (Lp).1 Lp is present in the environment – in soil and water – and survives and thrives in many potable hot water systems. Legionella infections only occur through direct exposure to aerosols/droplets from an environmental source colonised by the legionella bacteria – there are no reported or documented cases of Legionnaires’ disease associated with person-to-person transmission. Legionella grows in warm, stagnant water in natural and artificial water systems – in particular, cooling towers, evaporative condensers, hot and cold water systems and spa pools. These environments – as well as being ideal for growth – may also provide the means by which aerosols/droplets are generated and the organism dispersed into the atmosphere.2 So, a significant potential danger is at the point of hot water delivery, and there are numerous reports of Lp being present in 10% to 50% of sampled taps and showers in Europe and the United States.3 To provide an indication of the impact of UK exposure to legionella in recent years, the number of cases of legionellosis in the UK has remained reasonably constant, at between 300 and 400 per year, as shown in Figure 1 (with a slight, unexplained dip in 2011).
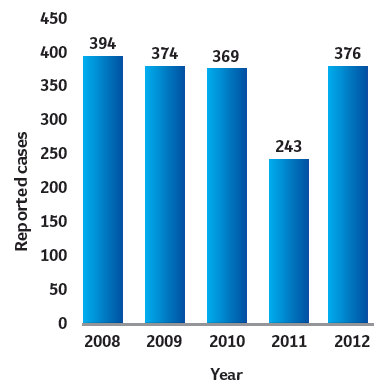
Figure 1: Number of cases of legionellosis reported in UK, 2008-2012 (Data source: Annual epidemiological report 2014. Respiratory tract infections4)
For the most recently available data – collected in 2012 – of the confirmed cases of Legionnaires’ disease, just over half were considered to have been due to exposure in the community and healthcare facilities, with the remainder being associated with travel abroad. This apparent figure of under 200 annual cases derived from a UK source is likely to be an underestimate5 of the true incidence of legionellosis, as symptoms are often similar to the influenza virus and other types of bacterial pneumonia, and routine laboratory tests will not readily identify the legionella bacteria.
The group at greatest risk from contracting legionellosis is older males with underlying health problems such as heart conditions and diabetes. The susceptibility of this group is thought to be associated with industrial occupations and lifestyle-related risk factors, such as smoking.2 The historic England and Wales fatality rate is just over 10% for community-acquired legionellosis and around 25% for nosocomial (healthcare) related. However, infections in the UK are erratic, and in many cases a specific source of infection is difficult to trace.
As identified in Figure 2, the legionella bacteria will multiply abundantly between the temperatures of 20°C and 46°C – a range that coincides with temperatures that are acceptable for supplying potable hot water. It is notable that ‘cold’ water services can often be in environments that allow them to rise to a high-risk temperature. The most favourable temperature for the multiplication of legionella is approximately 37°C. Above 70°C, the bacteria will be killed almost instantly, and at a temperature of 60°C, 90% of the legionella pneumophila have been shown to be killed in two minutes (compared with several hours at around 50°C). Below 20°C, legionella becomes dormant but ready to multiply when the opportunity presents itself.
Figure 3 shows the interesting effect that the thermal resistance of pipe insulation has in prolonging opportunities for non-flowing hot water temperatures to drop to the most critical temperatures. For the higher resistance, better insulation (shown as Type 1) keeps the water hotter for a longer period; but, as it cools, it will also mean that the water temperature will remain for a greater time in the range where legionella will multiply.
This problem in water distribution systems is exacerbated where there is accumulation of sludge, rust, scale and particulate deposits that act both as a haven for bacteria and, as biofilms develop, provide nutrients.
Approved Code of Practice L8 – Legionnaires’ disease. The control of legionella bacteria in water systems
In the UK, HSE L87 gives advice on reducing the risk from exposure to legionella bacteria. The L8 revision in 2013 removed the technical guidance (which was Part 2 in previous editions), and published this separately as HSG274.8 HSG274 outlines measures that, together, meet the relevant statutory safety requirements, including: identifying and assessing sources of risk; preparing a scheme to prevent or control risk; implementing, managing and monitoring precautions; keeping records of precautions; and appointing a manager responsible for others. This guidance is split into three parts that consider specific applications for the control of legionella bacteria: part 1 – evaporative cooling systems; part 2 – hot and cold water systems; and part 3 – other risk systems. These are all freely downloadable from the internet and provide extensive, essential, very practical, and well-illustrated guidance.
Prevention of opportunities for legionella proliferation during design
HSG274 part 2 provides comprehensive guidance for the design, commissioning and operation phases of a commercial hot water system. The recommended design aspects are abstracted below – more comprehensive details are available in HSG274 part 2.
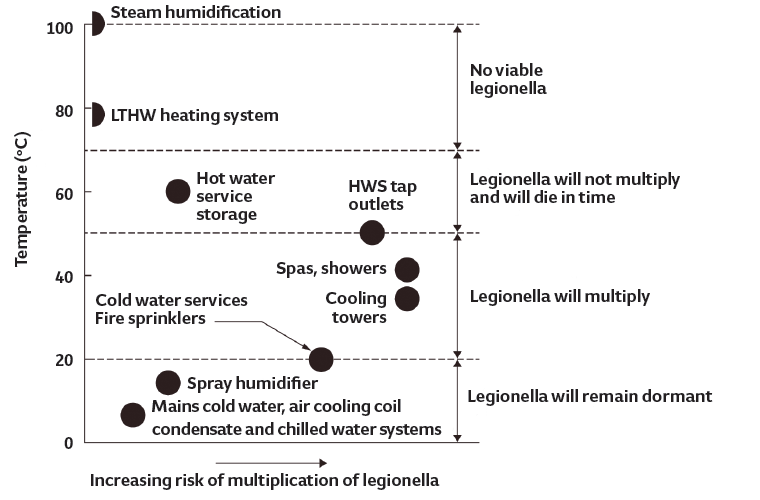
Figure 2: Typical system operating temperatures and the risk of legionella proliferation (Source: CIBSE AM13:201366)
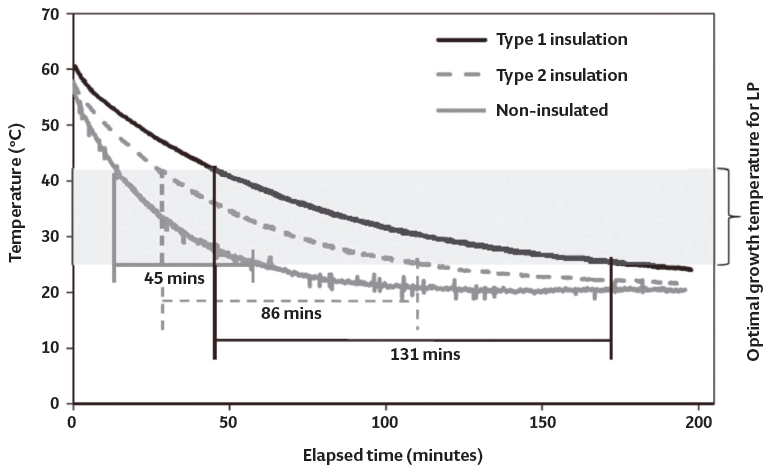
Figure 3: Heat loss during stagnation of hot water in 1.25cm diameter copper pipes, with and without insulation at room temperature (Source: Bedard3)
There should be an adequate supply of hot water, particularly at periods of peak demand, while avoiding excessive storage and ensuring a supply temperature of at least 60°C from the heat source and/or storage vessel (calorifier). In buildings where stored water is not ‘essential’, consideration should be given to direct mains systems – this could be provided through continuous flow hot water systems or ‘point of use’ heaters. Modular high output continuous flow hot water heaters are very capable of providing thousands of litres of hot water per hour, without the need for storage.
If a calorifier is employed, it should meet the normal daily fluctuations in hot water use, without any significant drop in target supply temperature. Also, the temperature in the base of the vessel should be monitored and must be drainable to remove accumulated sludge and particulate matter. The distribution system should be thoughtfully designed to avoid water stagnation by ensuring flow through all parts of the system, and particular care should be taken to prevent risk temperatures in system components that support microbial growth. Low-use outlets should, for example, be installed upstream of frequently-used outlets, to maintain frequent flow.
Hot water temperatures at an outlet should reach 50°C (55°C in healthcare premises) within one minute of turning on the tap. This will require a recirculation loop in most commercial systems that should be designed to give a returning temperature of at least 50°C (55°C in healthcare premises) – there should be temperature measurement points so that this may be monitored. Circulating pump design and the correct commissioning of balancing valves are key issues to ensure flow throughout all parts of the hot water system – particularly the hot water return legs – to avoid long lengths of stagnant pipework that are likely to be at a lower temperature
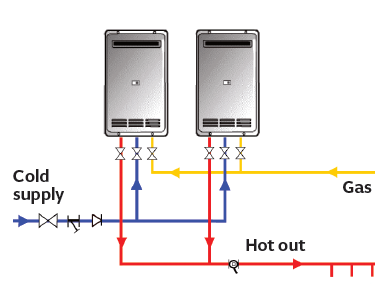
Figure 4: Continuous flow hot water system has no storage of hot (or warm) water, substantially
reducing the opportunity for any Lp growth (Source: Rinnai UK)
Where a traditional indirectly heated hot water calorifier is employed, cold water will typically enter at the base of the calorifier, creating an area below the coil where the initial blended water temperature may support microbial growth and provide potential breeding ground for legionella. This may be mitigated with a shunt pump to mix the water in the calorifier to ensure a temperature of at least 60°C is achieved throughout the vessel for at least one continuous hour a day. This will, unfortunately, reduce the energy effectiveness of the system.
All system materials chosen should reduce corrosion, prevent excessive scale formation and not readily support microbial growth. In hard water areas, softening of the cold water supply to the hot water distribution system should be considered – this can reduce the risk of scale being deposited, the risk of scale accumulation within the system pipework and components and, if used, in the base of the calorifier. The design should ensure reasonable access to all pipework sections and active system components for inspection and maintenance purposes, with valves located sensibly for practically useful isolation. Any energy efficiency or water conservation measures should be assessed carefully at the design stage, to ensure the control of legionella is not compromised.
Instantaneous water heaters
By using instantaneous water heaters, as shown in Figure 4, the potential legionella hazards inherent in stored water systems are avoided as – by design – they do not store any volume of hot water but are still able to supply large commercial demands. The incoming cold water is instantaneously heated to 60°C, beyond the temperature at which the bacteria can multiply, and that heated water is not resident in the hot water generating equipment for prolonged periods. Without the need for calorifiers or other storage vessels, the volume of hot water in the system is reduced and, as these systems do not include a standing store of water, they do not require a daily ‘pasteurisation’ cycle using shunt pumps.
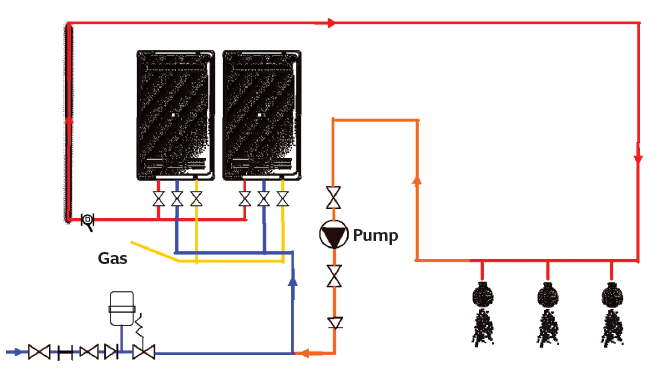
Figure 5: Continuous flow with recirculation (Source: Rinnai UK)
However, regardless of whether the hot water is provided by a continuous flow water heater, in larger systems – where there is a need for recirculation pipework (as illustrated in Figure 5) – there is inherently increased system water volume and opportunities for ‘dead-legs’. When taps or shower-heads stop running, after use, the final branch pipework will be full of cooling water capable of breeding legionella bacteria, so appropriate safeguards must be put in place – such as self-draining shower heads.

Figure 6: A pair of continuous flow water heaters installed to produce in excess of 1,400 litres per hour of hot water at 60°C (Source: Rinnai UK)
Water treatment
Water treatment for the cold water supply is an important consideration, especially in areas of hard water. Water quality is variable according to geographical location – for example, in England, water is typically harder towards the south and east, and softer towards the north and west. But there are local variations, depending on the physical source of the water. Hard water contains dissolved minerals – mainly calcium, magnesium and associated anions bicarbonate, sulphate and chloride. When hard water is heated, bicarbonate decomposes and calcium carbonate is deposited into the waterheater tank and associated pipework. Mineral deposits can dramatically reduce the efficiency of appliances and, eventually, cause the unit to fail. For example, a water-heater tank with a limescale coating of one-millimetre thick can equate to approximately 7% loss in efficiency.6 Water treatment should, of course, be properly considered with all types of hot water services, including continuous-flow water heaters and water heated indirectly using calorifiers.
Thermal disinfection
The hot water system – particularly rarely used shower heads or terminal fittings – will still require regular checking and disinfection. When the building is not in occupation – for example, weekends or at night – thermal disinfection of hot water services can be carried out by raising the temperature of the whole contents of the circulating water to 60°C (or above) for at least an hour. To meet the requirements of HSG274 thermal disinfection, every hot water outlet throughout the system must then be flushed and allowed to flow for five minutes at full temperature. To be effective, the temperature at the hot water generator should be maintained to ensure that the temperature at the outlets does not fall below 60°C. In the case of a storage calorifier, this could necessitate the whole volume of stored water being raised to a high temperature – beyond normal safe temperatures that prevent scalding at outlets – to undertake disinfection, then that stored water temperature would need to be reduced (or the water drawn off and discarded) before normal building occupation.
However, with a continuous flow system, such as in Figure 6, the electronic control is such that the temperature can be instantly raised – potentially, to beyond 75°C and within a tolerance of +/- 1K – to undertake disinfection. The temperature is controlled based on the incoming water to the continuous flow water heater and so, as with normal operation, it will modulate (typically down to around 50 watts), only consuming the energy required to meet the instantaneous flow requirements. Following the disinfection procedure, the flow temperature can then, just as swiftly, be returned to 60°C – ready for safe building operation.
© Tim Dwyer, 2015.
References
- Currie, SL, et al, ‘Legionella spp. in UK composts – a potential public health issue?’, Clinical Microbiology and Infection, Volume 20, Issue 4, April 2014.
- Legionnaires’ disease in England and Wales 2012, Public Health England, 2014.
- Bedard, E, et al, ‘Temperature diagnostic to identify high risk areas and optimize legionella pneumophila surveillance in hot water distribution systems’, Water Research, 71, 2015.
- ECDC Surveillance Report,Annual epidemiological report. Respiratory tract infections, 2014.
- Whiley, H, et al, ‘Uncertainties associated with assessing the public health risk from legionella’, Frontiers in Microbiology, September 2014.
- CIBSE TM13 Minimising the risk of Legionnaires’ disease, CIBSE, 2013.
- HSE L8 Legionnaires’ disease – The control of legionella bacteria in water systems, UK Health and Safety Executive, 2013.
- HSE HSG274 Legionnaires’ disease Technical guidance, UK Health and Safety Executive, 2013.


