
CPD sponsor
The very first requirement in a hospital is that it should do the sick no harm.’ – Florence Nightingale.
The UK government’s Spending Review in June 2025 announced £750m of funding for infrastructure repairs at more than 400 NHS hospitals, mental health units and ambulance sites. The opportunity exists to improve, where it is needed, ventilation systems across the healthcare estate.
Preventing airborne contamination, ensuring patient and staff safety, maintaining medical product integrity and achieving energy efficiency targets are essential outcomes from critical healthcare ventilation systems (CHV).
CHV systems are crucial for ensuring the safety of their respective areas. Health technical memoranda (HTMs) – and, specifically, HTM 03-01 Specialised ventilation for healthcare premises1 – provide the authoritative guidance, and compliance is paramount.
The areas defined by HTM 03-01 as needing specialised critical ventilation because of high risk include: ultra-clean ventilation systems, such as operating theatres; and isolation rooms, such as wards for patients with airborne infectious diseases.
HTMs distinguish mandatory, legally binding requirements (‘must’) from key best-practice recommendations (‘should’) that support their stringent standards. This guidance is critical for design, installation, operation and maintenance, and is applicable across the entire building life-cycle.
The HTM establishes a standard approach for identifying and labelling ventilation systems, as well as developing an inventory of installed systems.
The inventory will be arranged according to the following categories:
- Local exhaust ventilation systems (LEV)
- Critical healthcare ventilation systems (CHV)
- General ventilation systems (GVS)
- General extract systems (GES)
- Smoke clearance and heat exhaust systems (SHEVS).
The 2021 version of HTM 03-01 introduced the concept of the ventilation safety group (VSG) in healthcare organisations, which oversees the management of the healthcare provider’s ventilation systems and reports at board level. The HTM suggests a typical composition for a VSG, to ensure the necessary expertise is brought together to manage ventilation risks (see panel, ‘Disciplines in the ventilation safety group’).
Disciplines in the ventilation safety group (VSG)
The VSG should be a multidisciplinary group and, typically, comprise the following, according to HTM 03-01:
- Authorising engineer/independent adviser for ventilation
- Infection prevention and control nurse or specialist
- Authorised person(s) for ventilation services
- Estates (operations and projects) staff
- Clinicians and specialist departments (for example, theatres, critical care areas, pharmacy, medical microbiology, nursing, decontamination)
- Personnel from the finance department with accountability for capital and revenue evaluation
- Other stakeholders as appropriate
- Co-opted expertise (for example, ventilation designers, consultants and suppliers).
The primary driver in CHV systems is mitigation of airborne infection risks, particularly in sensitive areas such as operating departments, critical care facilities and isolation rooms. (See panel, ‘Airflow strategies for infection control’.)
Airflow strategies in healthcare premises
Positive-pressure rooms
Operating rooms, ICUs and pharmaceutical compounding areas, where sterile conditions are paramount, all require clean filtered air. Contamination of these spaces from ingress of contaminated air is prevented by maintaining the space at a positive pressure relative to adjacent spaces. This results in clean filtered air moving outwards from the room, preventing contaminants from entering
Negative-pressure rooms
In some situations, it is necessary to protect staff and other occupants against airborne organisms from patients with an infectious disease (for example, tuberculosis, Covid-19, measles, chickenpox). The ventilation system is used to keep the room at a lower internal pressure to the surrounding spaces and draws air inwards, containing the pathogens within the room and protecting surrounding areas and staff.
Dilution and scouring
Beyond pressure, precise airflow rates are essential for diluting airborne contaminants and efficiently ‘scouring’ spaces. In ultra-clean ventilation (UCV) operating theatres, high air velocity purges contaminants from the surgical zone, significantly reducing post-operative sepsis. This ensures staff operate in a ‘clean airflow path’ and medicinal product integrity is protected.
Energy efficiency
Modern designs use accurate measurement to optimise energy consumption, supporting net zero carbon targets through control strategies such as ‘setting back’ systems (reducing output when not in full use).
Poorly designed or maintained systems can become sources of microorganisms. Ventilation directly protects vulnerable patients from airborne organisms and fungal spores in rooms such as intensive care units and transplant units. It safeguards staff from anaesthetic agents, microorganisms and toxic substances.
Controlled environments are vital in pharmacy aseptic preparation facilities and sterile services departments, to ensure quality assurance and compliance with EU good manufacturing practice (GMP), which describes the minimum standard that a medicines manufacturer must meet in its production processes if its medicines are to be sold in the EU.
Airflow measurement is mandated by legislation such as the Health and Safety at Work etc. Act 1974 and Control of Substances Hazardous to Health (COSHH) Regulations 2002, which require statutory examination and testing of local exhaust ventilation at least every 14 months. Failure to maintain standards can lead to increased health risks and legal action.
HTM 03-01 states that all CHV systems will be inspected quarterly and verified at least annually. The purpose of verification is to determine if the system is performing to an acceptable level. Airflow and its measurement are clearly key to this annual verification, as well as the initial commissioning and the final acceptance validation.
Critical sensors for ventilation systems
Sensors are the ‘eyes and ears’ of a ventilation system, providing data for continuous monitoring, automatic control, alarm generation and data logging within the environmental monitoring system (EMS), which works independently using independent sensors in parallel with the building management system (BMS).
The accurate measurement of the quantity and condition of the air is crucial to maintaining the performance of the system and, hence, its role in infection control. The EMS sensors are calibrated to the appropriate standard and must have valid calibration certificates.
The air change rate is a crucial metric in healthcare ventilation. Accurate measurement and verification are essential to ensure compliance with required standards for each space. This will also be key to maintaining pressure differentials required between spaces. Sensors are essential for collecting this data and must be calibrated to the appropriate standards.
Differential pressure sensors
These are fundamental for recording or indicating air pressure differentials between adjacent rooms – crucial for contamination control. They verify positive pressure in sterile areas (for example, operating theatres) and negative pressure in isolation rooms.
The sensor has two ports connected by small tubes to the spaces being compared. It continuously monitors the pressure difference and sends a signal to the EMS. If the pressure deviates from the required setpoint (often around +10 to +15Pa), alarms can alert the operators. The maintenance team shall be alerted to rectify the automatic control system.
For example, HTM03-01 states that they should be used to indicate to the operating theatre control panel if the ultra-clean ventilation (UCV) canopy falls below 80% of its design flowrate.
Direct-reading Magnehelic mechanical gauges, with green and red indicators for differential pressure ranges, are required at critical points.
Electronic pressure transducers (such as those manufactured by CMR Controls) are sensors that convert the force exerted by the air into a measurable electrical signal (voltage/current or digital). They feed continuous data to the EMS for automated monitoring, plant failure, low airflow and ‘filter fault alarms’. Plant failure and low airflow alarms should be indicated when the air quantity falls below 80% of the design value.
Airflow/volume/velocity sensors

Figure 1: A P-sensor ultra-low air pressure and air volume sensor (Source: CMR)
These are electronic devices that measure and quantify the movement of air, providing the critical data needed to monitor, manage, control and optimise ventilation and process systems.
These are essential for measuring air volume and velocity in systems, and to ensure adequate dilution and ‘scouring’ in spaces.
In UCV theatres, they confirm the high air velocity needed to purge surgical zones. It is normally expressed as air-change rate. Methods of measuring velocity include veloprobes, flowgrids, pitot tubes and manometers for ducts, thermal anemometers for precise velocity, and calibrated hoods (balometers) for terminal air volumes.
HTM03-01 states that ventilation system performance should be measured at the main and branch duct test points with either a pitot tube or a thermal manometer. Accurate and meaningful duct measurements depend on using the correct method, including proper spacing of – and the appropriate number of – measurements across the ductwork cross-section.
It is essential to fully recognise this, as inaccurate data collection may result in – and subsequently hinder the identification of – performance issues. CPD modules 61 and 235 give more background on in-duct measurements in ventilation systems.
Plug and electronically commutated (EC) fans often have a measuring ring for direct output readings.
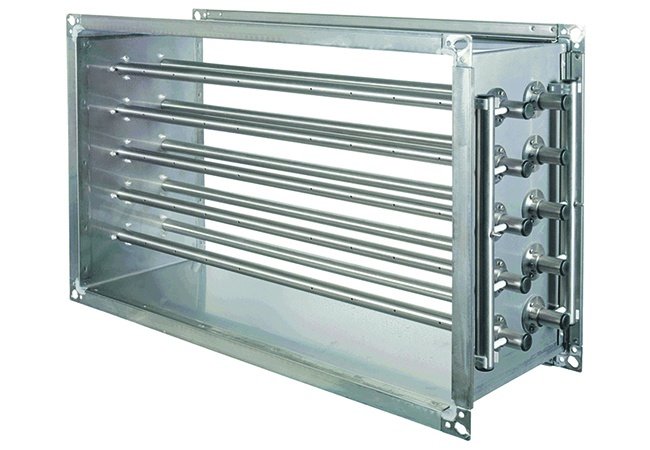
Figure 2: Flowgrid air volume measurement system (Source: CMR)
Temperature sensors
These monitor room and supply air temperatures to maintain comfort and prevent detrimental conditions for patients or equipment. Actively ventilated sensors are preferred in critical areas such as operating theatres. In these situations, the sensors would be located in a sampling duct mounted on or adjacent to the theatre control panel, or in one of the theatre’s low-level extract ducts.
Humidity sensors
These monitor relative humidity to prevent condensation and mould growth, and maintain specific environmental conditions. While acknowledged as prone to inaccuracy, they are important for applications such as pharmacy cleanrooms.
Clearly, the accuracy of the instrumentation and its correct placement in the ventilation system is key to delivering the required performance standards.
Commissioning, validation and control
The VSG’s remit includes the commissioning and validation processes for ventilation systems. Proper commissioning and validation are essential for ensuring that systems function effectively to support patient and staff safety.
Sensor data is vital for commissioning, which brings systems to an operating condition, ensuring they meet design specifications and fall within their range of acceptable tolerances. The measurement equipment should have valid calibration certificates that are traceable to the appropriate standard
HTM 03-01 reinforces the point that in-duct measurement positions should be identified at the design stage. This should result in the correct placing of testing and measurement devices, resulting in accurate measurement. These positions will need to be accessible for commissioning and annual verification of the system performance. Addressing these issues during design ensures precise placement of measurement facilities.
Independent validation is undertaken on the completion of the commissioning processes. Independent validation assesses the ‘fitness for purpose as a whole’ of the entire installation, including building fabric and system performance.
It is important to note that the validation process is not a ‘snagging’-type exercise. The system offered for validation is done so on the basis that it is fully complete, commissioned and achieving the required performance. The validator needs to be a suitably qualified competent engineer and independent of the system designers, contractors, suppliers, installers and commissioners. Calibration certificates must be issued to verify the accuracy.
The records on system performance generated during the validation process, and the ongoing information from the annual validation, are a legal requirement. The information needs to be in a form that can be readily accessed. HTM 03-01 Part A section 13 gives details of the required information to be stored and recorded.
Independent of the EMS sensors, ventilation system sensors enable real-time control adjustments via BMS, and can trigger alarms for plant failure or low airflow. This can ensure ongoing safe and efficient operation in live time, further supporting the delivery of patient and staff safety beyond the essential annual verification process.
Updating and managing healthcare ventilation infrastructure
Simon Everett’s2 research paper examines the difficulties involved in managing legacy ventilation systems within current healthcare estates. His paper gives a good overview of the situations faced by estates teams, including financial limitations, how to prioritise upgrades, the importance of the annual verification reports, and the overseeing of the ventilation systems by the VSG.
The paper makes the point that, if the annual verification indicates the system is not performing to the required standard – and, hence, ‘should not be returned to service’, as the HTM states – then this should generally not be a surprise to the senior leaders in the healthcare organisation (although he states it often is), as the VSG should be aware of ongoing life-cycle issues and have mitigation measures in place.
The reliable acquisition of accurate airflow measurement data verified by traceable calibration certificates is fundamental to the function and management of CHV systems
Accurate data will support ongoing work and management to ensure patient and staff safety, maintaining medical product integrity and achieving energy efficiency targets, the essential outcomes from CHV. Ultimately, precise airflow data underpins patient safety, operational efficiency and compliance.
© Gordon Hudson, 2025.
About the author
Gordon Hudson is an independent consultant and CIBSE trainer. He also presents the Vintage Sustainability podcast – bit.ly/CJVSGH
References:
1 Health Technical Memorandum 03-01: Specialised ventilation for healthcare premises – bit.ly/4mSQPyE
2 Everett, S D, (2024), ‘Managing critical systems is often a challenging risk’, Health Estate Journal, vol 78, issue 8, pp. 67-70 – bit.ly/4ofZjBn
